Osteoarthritis of the hip (HJ) is a degenerative-dystrophic disease that affects cartilage and bone tissue. In medical articles, it can be called another way: coxarthrosis deformity, DOA of the hip joint, osteochondrosis. All these terms mean the same pathology - joint disease, but "coxarthrosis" is a narrower concept that characterizes the failure of the hip joint.
Cartilage is the first part of arthritis, then bone and surrounding structures - ligaments and muscles - participate in the pathological process. If there are changes in the bones, the prefix "osteo" is added to the word "arthrosis". In advanced cases, the joint was deformed, and they talked about joint deformity (osteoarthritis).
General features
Deformed hip osteoarthritis is the second most common disease after osteoarthritis of the knee. Due to the deep position of the hip joint, the bone deformity may not be noticed for a long time, only the X-ray at the later stage can see the change.
The development of this disease is influenced by various factors, including a sedentary lifestyle, trauma, and metabolic disorders. It is because of the peculiarities of modern life, in which there is often no place for physical education, that joint disease affects more and more people. Moreover, the highest incidence falls in the middle age group - from 40 to 60 years old.
Authority to solve:coxarthrosis usually affects women more than men.
Development Mechanism
The thigh joint is formed by two bones: the femur and the pelvis (pelvis). The head of the femur enters the pelvic joint, immobile during movement - walking, running. Simultaneously, the articular surface of the femur can move in multiple directions, providing the ability to flex, extend, abduct, add, and rotate (rotate) the thigh.
During physical activity, the femur moves freely within the femur joint because of the cartilage tissue that covers the joint surfaces. Hyaline cartilage is distinguished by its strength, solidity and elasticity; it acts as a shock absorber and participates in the distribution of loads during human movement.
Inside the joint is the synovial capsule - the substance needed to lubricate and nourish the cartilage. The entire joint is enclosed in a dense, thin capsule surrounded by powerful muscles in the thighs and buttocks. These muscles, which also act as shock absorbers, prevent injury to the hip joint.
The development of coxarthrosis begins with changes in the joint fluid, which becomes more viscous and denser. Due to a lack of moisture, the cartilage does not receive enough nutrition and begins to dry out, lose its smoothness, and cracks appear on it.
Bones can no longer move freely as before and rubbing against each other causes micro-damage in the cartilage. The pressure between the bones increases, the cartilage layer thins. Under the influence of increasing pressure, bones are gradually deformed, local metabolism is interrupted. In the later stages, there are obvious signs of leg muscle atrophy.
Reason
Hip deformity can be primary and secondary. It is not always possible to determine the cause of primary joint disease. Secondary arthropathy appears against the background of existing diseases, namely:
- congenital hip dislocation or hip dysplasia;
- Perthes disease (aseptic necrosis of the femoral head);
- hip arthritis of infectious origin, rheumatic or other causes;
- pelvic trauma - dislocation, fracture.
Hip dysplasia is a congenital malformation that sometimes goes undiagnosed for a long time and in the future (ages 25–55) can lead to the development of dysplastic coxarthrosis.
Coxo arthrosis can be left, right, and symmetrical. In primary rheumatic disease, concomitant diseases of the musculoskeletal system are often observed - in particular, osteosarcoma and gonarthrosis.
There are also risk factors that contribute to the onset of the disease:
- excessive weight and excessive loads overload the joints;
- violation of blood circulation and metabolism;
- hormonal changes;
- curvature of the spine, flat feet;
- advanced age;
- lower motivation;
- heredity.
It should be noted that coxarthrosis itself is not hereditary. However, certain features of the metabolism or the structure of the connective tissues can set the stage for the future development of arthropathy in a child.
Symptoms of coxarthrosis
The leading symptom of degenerative hip disease is hip and groin pain of varying intensity. Stiffness and stiffness on movement, decreased muscle mass, shortening of the affected limb, and altered gait due to limping have also been reported.
Coxarthrosis most often progresses slowly, causing discomfort at first and mild pain after exertion. However, over time, the pain increases and appears at rest.
A typical manifestation of the pathology is difficulty flexing the hips, when a person cannot sit "crouched" in a chair. The presence and severity of signs of coxarthrosis depends on its severity, but pain syndrome is always present.
There are three degrees or forms of arthritis of the hip, which vary in severity of injury and accompanying symptoms:
- 1 degree. Thighs don't hurt all the time, but cyclically, mostly after walking or standing for a long time. The pain is localized to the joint, but can sometimes radiate down the leg to the knee. Grade 1 muscle spasms do not decrease in size, gait does not change, mobility is fully retained;
- Grade 2. More intense pain, arising not only after running or walking, but also at rest. The pain is usually concentrated in the thigh area, but can radiate down to the knee. In times of heavy lifting, stepping on the injured limb is very painful, so the patient begins to lose his leg and limp. Decreased range of motion in the joint, especially with difficulty moving the leg to the side or turning the hip;
- 3 degrees. The pain is frequent and does not subside even at night. The gait is markedly impaired, independent movement is significantly complicated, and the patient has to rely on a cane. The range of motion is severely limited, the gluteal muscles and the entire leg, including the lower leg, atrophy.
- Due to muscle weakness, the pelvis is tilted forward, the affected leg shortens. To compensate for the difference in length of the limbs, the patient leans on the affected side when walking. This leads to a shift in center of gravity and increased stress on the affected joint.
Osteoarthritis or Osteoarthritis?
Arthritis is inflammation of the joints, which can be an independent disease or develop against a background of systemic disease (eg, rheumatic disease). In addition to the inflammatory response, symptoms of osteoarthritis (especially in the advanced stages) include limited range of motion and changes in the shape of the joints.
Central to the degenerative-dystrophic changes in arthropathy is the failure of cartilage tissue, which often leads to the appearance of inflammation. That's why joint disease is sometimes referred to as ankylosing spondylitis. And since osteoarthritis is almost always associated with joint deformity, the term "osteoarthritis" is applied to it.
Authority to solve:According to the International Classification of Diseases (ICD-10), osteoarthritis and osteoarthritis are varieties of the same pathology.
Diagnosis of coxarthrosis
The diagnosis of "coxarthrosis of the hip" is made on the basis of examination, patient complaints and examination results. The most informative method is X-ray: in the picture you can see both the extent of the joint damage and the cause of the disease.
For example, in hip dysplasia, the tibia is flatter and steeper, and the cervico-diaphyseal angle is greater than normal. Deformation of a portion of the femur located in the vicinity of the joint is characteristic of Perthes disease.
Grade 3 coxarthrosis is characterized by narrowing of the joint space, enlargement of the femoral head, and multiple growths (osteoblasts).
If the patient has a fracture or dislocation, signs of injury will also show up on the x-ray. If detailed evaluation of bone and soft tissue condition is required, magnetic resonance imaging or computed tomography may be indicated.
Differential diagnosis is carried out with the following diseases:
- gonarthrosis;
- osteonecrosis and lens syndrome arise against its background;
- trochanteritis (inflammation of the trochanter bone of the thigh);
- ankylosing spondylitis;
- reactive arthritis.
Loss of muscle volume associated with grade 2 and 3 spasticity can cause knee pain. Furthermore, the knee often hurts more than the hip joint. To confirm the diagnosis and rule out gonarthrosis, an x-ray is usually sufficient.
With diseases of the spine - osteonecrosis and pinched nerve roots - the pain is very similar to coxarthrosis. However, it happens suddenly, after an unsuccessful move, a turn, or lifting weights. The pain starts in the buttocks and spreads down the back of the leg.
Lens syndrome is characterized by severe pain when lifting a straight limb from a supine position. However, there is no difficulty in collapsing the leg to the side, as with coxarthrosis. It is important to note that osteonecrosis and hip osteoarthritis are often diagnosed at the same time, so a comprehensive examination is required.
Appendicitis, also known as pulmonary bursitis, develops rapidly, in contrast to joint disease, which can progress slowly over years and even decades. The pain syndrome develops within a week or two, while it is quite intense. Colitis is caused by trauma or overuse. Movement is unrestricted and legs are not shortened.
Ankylosing spondylitis and reactive arthritis may also be accompanied by symptoms that mimic coxarthrosis. The telltale sign of these diseases is the appearance of pain mainly at night. The hip can be quite painful, but with walking and movement, the pain should subside. In the morning, the patient worries about stiffness, which disappears after a few hours.
Treatment of hip arthritis
Coxarthrosis can be cured conservatively or surgically. The choice of treatment method depends on the stage and nature of the pathological process. If diagnosed in grade 1 or 2 of the disease, it is treated with medication and physical therapy. After the relief of acute symptoms, therapeutic exercises and massage will be added to them. If necessary, a special diet is prescribed.
The earlier coxarthrosis is detected and treated, the more favorable the prognosis. With the help of drugs and treatment measures, you can significantly slow down the pathological process and improve your quality of life.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to reduce pain and inflammation. It should be borne in mind that anesthesia is carried out for the shortest possible time, since drugs of the NSAID group can negatively affect the gastrointestinal tract and slow down the regeneration process in cartilage tissue.
It is possible to speed up the recovery of cartilage with the help of chondroprotectors. However, these funds are effective only in the early stages of the disease, when its hyaline cartilage has not been completely destroyed. Chondroprotectors are prescribed in the form of tablets or intra-articular injections.
To improve the blood supply to the joints, vasodilators are used. For muscle spasms, muscle relaxants are recommended.
In cases of persistent pain syndrome that is difficult to eliminate with pills, an injection is given into the hip joint. Corticosteroids help reduce inflammation and provide good pain relief.
Drug therapy can also be supplemented with topical agents - ointments and gels. They don't have a noticeable effect, but they help deal with muscle spasms and reduce soreness.
Physical therapy helps to improve blood circulation and cartilage nutrition. For coxarthrosis, procedures such as shock wave therapy (SWT), magnetic therapy, infrared lasers, ultrasound, and hydrogen sulfide baths have proven themselves to be excellent.
Work
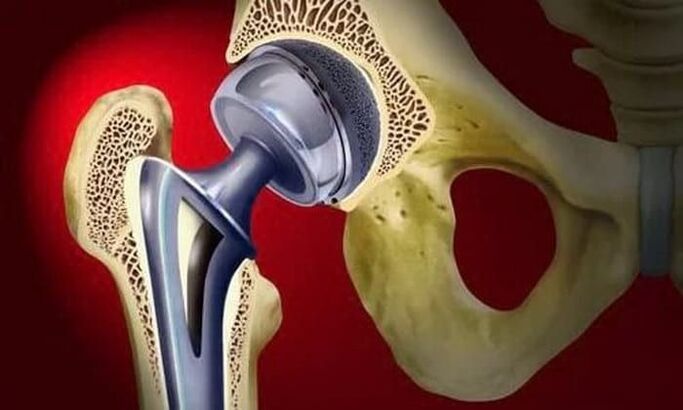
Treatment of stage 3 osteoarthritis can only be surgical, because the joint is almost completely destroyed. To restore function of the hip joint, partial or total arthroplasty is performed.
Surgical treatment is applied in cases of advanced osteoarthritis, when conservative therapy is not effective.
In partial prostheses, only the head of the femur is replaced by an artificial prosthesis. Total prostheses are meant to replace both the femoral head and the tibia. The surgery is performed under general anesthesia, and in the majority of cases (about 95%), function of the hip is fully restored.
During the rehabilitation period, the patient is prescribed antibiotics to prevent infectious complications. The sutures were removed on days 10-12 and exercise therapy was initiated. The attending physician helps the patient learn to walk and correctly distributes the load on the operated limb. Exercise is an important step in increasing muscle strength, endurance, and elasticity.
The ability to work is restored on average 2-3 months after surgery, but for the elderly this time can be up to six months. After completing rehabilitation, patients can fully move, work and even play sports. The lifespan of the restoration is at least 15 years. To replace a worn-out prosthesis, a second surgery is performed.
Effect
Without prompt and adequate treatment, coxarthrosis can not only significantly worsen quality of life, but can also lead to disability and disability. Already in the second stage of arthropathy, the patient was placed in the third disability group.
When shortening the affected limb by 7 cm or more, when a person moves only with the help of improvised means, the second group will be assigned. The first group of disabilities is patients with grade 3 coxarthrosis, accompanied by complete loss of mobility.
The indications for medical and social examination (MSK) are:
- long course of joint disease, more than three years, with frequent exacerbations. Frequency of exacerbations at least three times every 12 months;
- undergoing laparoscopic surgery;
- severe disorders of musculoskeletal function of the extremities.
Preventive
The main ways to prevent coxarthrosis are diet (if you are overweight) and regular, but moderate physical activity. It is very important to avoid injury to the pelvic area and hypothermia.
When risk factors for developing joint disease are present, as in all patients with diagnosed disease, swimming is beneficial. Sports such as running, jumping, soccer and tennis are not recommended.



























